WHY ADDICTION TREATMENT DOESN’T WORK
Decades of research on treatment approaches along with understanding of human biology and psychology combine to invalidate the core components of “addiction treatment” in the U.S.
by Clark Miller
Published August 30, 2018
Updated April 6, 2021
"What we simply need is a a nice bulldozer, so that we could level the entire industry and start from scratch . . . There's no such thing as an evidence-based rehab. That's because no matter what you do, the concept of rehab is flawed and unsupported by evidence."
- Dr. Mark Willenbring, former director of treatment and recovery research at the National Institute of Alcohol Abuse and Alcoholism (NIAAA)
Community mental health and addictions outpatient treatment programs utilize the same elements that are found in “rehab”, or traditional residential treatment, all predicting at best no benefit, or harm:
Disease model
12-Step, Alcoholics Anonymous orientation
Group modality versus individual therapy
Treatment provided generally by “addiction professionals” unqualified to treat behavioral health conditions - with as little as two years of training - for example Certified Alcohol and Drug Counselors (CADC), and Chemical Dependency Professionals, (CDP)
Critiques and condemnations of these systems and the inadequacy of care provided are longstanding and commonplace: take-downs of a failed addiction treatment industry that is at best ineffective or harmful that have come in a steady stream for years, for example: here, here, here, and here, here, on websites, in books, in feature major media reports, in this ABC news special aired 15 years ago.
This remarkable film, “The Business of Recovery” documents and accurately portrays Treatment as Usual (TAU) provided Americans trapped in substance use epidemics as a criminal scam with oversight provided by medical model and governmental health regulators, no peer-reviewed evidence to support benefit, and normalized in popular culture by the sheen of decency and legitimacy awarded criminal organizations like Hazleton and the Betty Ford Center. Take a look at the trailer:
In other and upcoming posts we’ll take a closer look at the history of and lack of research to support TAU, as well as longstanding research from a variety of fields within behavioral health – including developmental biology, psychology practice theory, research on trauma and ACE, and other areas – that invalidate TAU as ineffective or worse.
Here, let’s take a more general look at the four core components defining TAU in rehab and essentially universally in outpatient addictions and mental health treatment programs in the U.S. - disease model; 12-Step; group modality; unqualified staff providing treatment – and how those components predict lack of benefit, harm, and continuation of the substance use epidemics vulnerable Americans are trapped in.
I - Diseased Brains ?
In precisely the same ways that abdication of critical thought, professional responsibility to do no harm, and of evidential and ethical reasoning led to creation by the medical industry of the predictable, avoidable, and lethal Opioid Crisis, TAU for problem substance use in the U.S. has been driven by fabricated “knowledge” and evidence-free medical understanding that predicts failed treatment outcomes and harm.
As summarized in a previous post - A runaway national substance use problem is not just worsening, but is a recognized crisis and epidemic that:
Impacts children as well as adults
Will increasingly overwhelm public health care resources
Has not benefited from or been moderated by $ billions and decades of research under a never-evidenced, fabricated “medical model”, nor by treatment as usual (TAU) that is not treatment at all, nor by “addiction medicine"
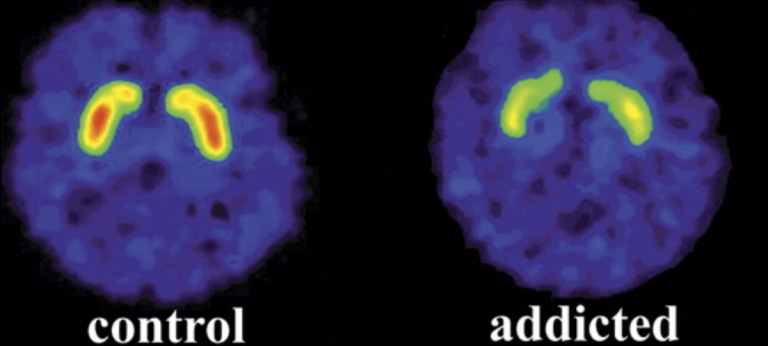
But it’s not just the lack of gains and worsening public health epidemic despite decades and $billions in public resources hijacked by the medical model that dismantles it as fiction. In a companion post the disease or “hijacked brain” model of substance use is dismantled, with links to primary research, as being invalidated by all relevant lines of research including longstanding epidemiological studies, logic, and the nature and course of relapse.
And in a relationship and combination that can only be described as bizarre, the medical industry’s fictional “brain disease” model - driving treatment and use of public healthcare funds for decades – has been coupled almost universally in “treatment” programs with a dominant “treatment model” that relies on the 50-year-old, very odd prescriptions and practice of a religious subculture, those practices invalidated by decades of research (below).
For a “disease of the brain”.
As is said at times, “You just can’t make this stuff up.”
The “hijacked brain” and other medical or disease model variants have driven addiction treatment for decades including diversion of enormous amounts of research resources – predicting at least some strong research evidence for effectiveness of medical approaches under those fabricated models if they are to any significant extent valid.
There is no such body of supportive research, instead: decades of multiple lines of invalidating theory and research, worsening national substance use epidemics, and continued diversion of public resources to those fictions.
II - What about the 12 Steps and AA – Alcoholics Anonymous ?
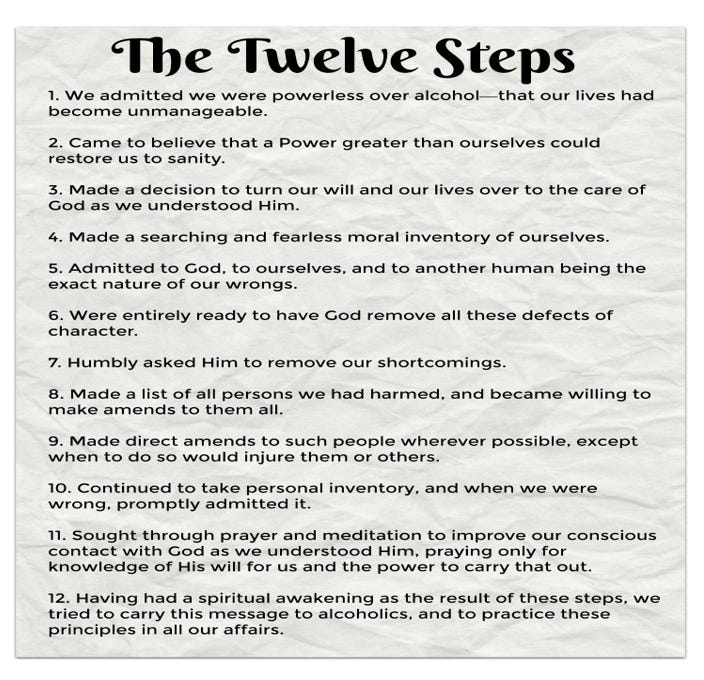
There is not now, nor has ever been, a body of scientific research to support the near-universal belief that participation in AA provides some type of beneficial effect for individuals struggling with compulsive, problem substance use, let alone has saved millions as is often asserted.
That is, the dominant substance use “treatment model”, like its companion medical or disease model of cause or “etiology”, is evidence-free, entirely unsupported by research, predicting at best no benefit, more likely harm by return to problem substance use. Treatment failure and steadily worsening substance use epidemics were, like the opioid crisis, predictable all along.
The constructed fabrications represent no form of scientific knowledge or evidence-driven understanding but instead Doxa – make believe knowledge fabricated to protect and maintain power, rewards, and status for those with the cultural capital to create and effectively message those fictions.
Over the course of going on two decades of direct practice with patients struggling with problem substance use and other mental health disturbances, I’ve listened to a number of them express with certainty that it was the “spiritual program” they worked in AA, the 12 Steps, and coming to know a Higher Power that saved them, provided a life of sobriety and good health.
About an equal number of patients seen are certain that accepting a Christian God, coming to know “the Lord my savior” is what cured them of problem substance use, or depressed mood, or other ailment. In fact, millions of Americans would confidently make that claim (just as thousands are certain that participation in AA was helpful to them).
Their confident reports have not led me, as an ethically-practicing therapist, to join in Christian prayer with patients, or to attempt to lead them to The Lord, or attempt to lead them to believe that engagement in the prescriptions and beliefs of organized religious practice will provide benefit to them. If I were to do that, I would hope that reports to my licensing board would result in revocation of my license and ability to practice, as a way to prevent harm to vulnerable patients.
Despite decades of heterodox voices
exposing the fiction of 12-Step practices as providing benefit, (some examples here, here, here, here, here and here) the very odd prescriptions of this religious subculture remain the dominant “treatment model” for substance use treatment in the U.S.
This assault against public health remains a tragic, criminal scam that exists partly as a way to perpetuate a massive entitlement system providing employment to individuals who are not qualified to provide validated treatment for substance use problems, but are often or generally aligned with and able and willing to recite and convey the empty and countertherapeutic (= predicting harm) platitudes of the religious programming of AA and The 12 Steps and to encourage or compel participation by patients in the religious subculture meetings. Individuals, that is, who are willing to practice unethically in ways that predict harm.
They became integrated in a substance use treatment industry historically infused with the culture, values, and managers and staff aligned with and involved in 12-Step religious culture, and were awarded positions largely by virtue of their allegiance to that subculture.
With 12-Step religious subculture constructed as a type of “treatment”, the lucrative, criminal, for-profit treatment industry can pay next-to-nothing for staff salaries, to individuals entirely unqualified to treat the complex, life-threatening conditions, generally in group treatment settings boosting billable services per staff member, and with no predicted benefit for clients, instead predicted perpetuation of problem substance use and epidemics.
Many professionals with experience and histories of employment in the treatment industry will attest to environments in which the “acid test” for employment or at least acceptance and integration with programs and staff requires endorsement if not participation in 12-Step related practices, culture and norms, and allegiances.
the dominant substance use “treatment model”, like its companion medical or disease model of cause or “etiology”, is evidence-free, entirely unsupported by research, predicting at best no benefit, more likely harm by return to problem substance use
And there is little sign of appreciation of the irony of AA’s cofounder Bill Wilson’s early death being related to addictive use of tobacco, still normalized in AA subculture, or of personal accounts of his use of AA meetings to prey sexually on vulnerable women coming into the program, a “tradition” currently known as “13-Stepping” and at odds with the trauma-informed care necessary for effective treatment of substance use problems.
An essentially overlooked social and public health pathology and cost
of AA and 12-Step religious subculture are the messages to acolytes attending meetings that normalize, enable, and reward continuing problem substance use, “addiction”, of arguably the most addictive and lethal substance sapping public health funds – tobacco.
Exposure to meetings of those religious subcultures places vulnerable individuals in settings where continued addictive use of tobacco is promoted by:
Normalization of smoking as something other than problem substance use
Celebration of tobacco dependent individuals as “clean and sober”
Ritualized group use of tobacco at meeting breaks, providing social reinforcement
Exposure to psychological associations, “triggers” for continued use
Continued use of tobacco predicts increased risk : of chronic pain; associated misuse and dependence on opioid pain medications; return to problem substance use, especially of alcohol and opioids.
The two systems, medical and 12-Step religious subculture, are fundamentally natural allies, partners, providing mutual support and - in effect - referrals, and each providing demonstrably false hope for Americans trapped in lethal substance use epidemics – one the false hope of a magical Higher Power and odd religious prescriptions providing benefit for a lethal behavioral disorder, the other the falsified and false hope of magic potions as treatment for a behavioral, psychosocial condition.
12-Step religious subculture and its very odd and countertherapeutic (= predicting harm) practices and prescriptions has driven addiction treatment for decades – predicting generation over that extended period of at least some strong research evidence for effectiveness to the extent that 12-Step practices and participation have some significant degree of validity as a benefit.
There is no such body of supportive research, instead decades of multiple lines of invalidating theory and research, worsening national substance use epidemics, and continued diversion of attention, treatment resources and program and policy development away from the longstanding evidence-based practices established for conditions driving the behavior of problem substance use.
III - The Lethal Myth of Group Treatment
In related and upcoming posts, we’ll take a closer look at the research and evidence establishing group treatment as an essentially ineffective type of treatment for problem substance use. Here, let’s outline the evidence and invalidating considerations.
There is no evidence base to support widely-used self-help, “process group”, or “check-in” groups as having any benefit.
Despite the privileged status of group modality (“group treatment”) in the folklore of substance use treatment and popular culture, and appeal to profiteers of greatly reduced costs of “treatment” (one paid employee to provide a billable service to 10 - 12 patients at once), group modality is not supported by evidence as effective with very limited exception (e.g. here; and in upcoming posts).
Evidence-based therapies supported as effective for compulsive substance use are individual modality therapies, provided by advanced level (licensed) behavioral health clinicians (upcoming posts).
More fundamentally, the myth of group treatment as an effective form of treatment for substance use and other problems is invalidated by the little known yet longstanding body of evidence establishing the primary role of the “common factors” in benefit provided generally to patients engaging in behavioral health services.
The “common factors approach”, or Contextual Model of Psychotherapy, marshals longstanding evidence to establish a fundamental fact in the provision of behavioral health services, or therapies – that based on decades of research, it is not any “specific factor”, like a therapy technique or protocol, but instead the factors common to any effective therapeutic interaction between a patient and behavioral health professional that largely predict success for the patient seeking relief and change.
Those “common factors” are the intangible yet crucial qualities of the interaction and “therapeutic alliance” that is established between a behavioral health provider and patient over the course of individual sessions and includes qualities experienced by the patient including: sense of safety; sense of authenticity (realness) of the therapist; sense of lack of judgement by the therapist, instead unconditional positive regard; close connection and sense of being cared about and understood by the therapist; sense of being able to trust and become vulnerable with the therapist, without fear of risk of emotional harm; sense of respect of patient’s autonomy, or choice; of patient’s dignity; of patient’s competence and right to collaborate in and choose direction of treatment.
Those factors – predicting the large share of beneficial effect in any behavioral health therapy interactions - emerge over a period in individual therapy sessions, NOT group therapy sessions. The extensive research establishing the common factors as the fundamental and crucial therapeutic factors in successful behavioral health treatment is based on patient outcomes in individual sessions with therapists, not group sessions.
Summing up so far -there is no research base for the provision of group therapy in substance use or other behavioral health treatment, with very limited exception – but crucially, providing and billing for ineffective behavioral health “treatments” maintains and increases profits for the medical and health insurance industries.
Provision of “treatments” without indication of benefit for life-threatening conditions predicts mortality and other harms.
It’s Not Just Common Factors Approach That Generally Invalidates Group Treatment
The somewhat dated and limited evidence for any benefit from group modality in substance use treatment is challenged by established and increasing evidence and practice theory linking problem substance use generally to chronic inner distress and deficits in emotional regulation linked to history of trauma and/or adverse childhood experiences (ACE), participation in such groups inconsistent with trauma-informed care. For example, key diagnostic features of Posttraumatic Stress Disorder (PTSD) include anxiety and hyperarousal with impaired attention and learning in novel and complex social settings. Moreover, very few patients are willing and comfortable working therapeutically on history of trauma in a group setting.
Evidence based therapies for addressing those effects are individual modality therapies provided by licensed mental health therapists, and the common effects of history of ACE and adult trauma – including fearfulness in novel and social settings, with impaired concentration and learning, and avoidance accessing and expressing difficult inner material – all contraindicate group modality.
Further, the presumed value of training for “relapse prevention skills” in group modality is increasingly undermined by the research evidence, which points away from social pressure to use substances and urges to use, per se, as predictors of relapse, and to other factors instead triggering relapse, most strongly: belief in the falsified “disease model” of addiction; deficits in self-efficacy; and situational stressors that are individualized and contextual, requiring individual modality exploration and therapies (upcoming posts).
IV - Unqualified Professionals Provide "Treatment" in a Multibillion Dollar Criminal Treatment Scam
With compulsive use of mood-altering substances (“addiction”) driving a steadily worsening public health crisis, highly lethal, the standards and regulations controlling what types of healthcare professionals are qualified and allowed to treat the lethal conditions based on their levels of training, competence and credentialing should be clear and reassuring –
but you don’t want to know.
Actually you do want to know and need to know, because it's a life and death matter. See this companion post - “Addiction: a Complex, Life-Threatening Behavior and Worsening Lethal Epidemic, with Treatment Provided by . . . No, Seriously”.
If licensed medical professionals in primary care settings were replaced by Medical Assistants - the medical team member who takes you to an exam room and gets your "vitals" - to diagnose, clinically formulate, and treat complex, life-threatening conditions, we would confidently predict horrific negative outcomes for public health due to that criminal behavior.
Think about it.
There is No Such Thing as “Addiction"
Most fundamentally addiction treatment fails because, as explained here in a related post, there is no such thing as “addiction” – no medical condition, no psychiatric disorder, no condition at all – because compulsive substance use is a behavioral symptom of something else, of underlying distress, unmet needs, and distorted, self-defeating beliefs, those complex sets of inner drivers as unique, numerous and variable as there are individuals, with their individual histories, circumstances and stressors, who struggle with problem substance use. That requires – demands – for effective treatment the comprehensive and thorough assessment and clinical formulation of each individual’s history, environment, social world, and inner life.
Effective treatment follows that assessment with evidence-based behavioral and psychological therapies provided by qualified behavioral health professionals. That picture of problem substance use and its treatment is fully aligned with what informs us from the extensive bodies of research related to trauma, especially adverse childhood experiences (ACE) and associated developmental neurobiology.
We know that compulsive substance use is a symptom of underlying distress as surely and as confidently as we know that patients exhibiting pain behaviors (for example wincing, grimacing, shifting positions, expressing pleas for relief, restricting movements and activities, etc.) and who explain to us that those behaviors are compulsive and represent their reflexive reactions to the inner experience of perceived pain – truly are experiencing pain and compulsively engaging in the symptomatic behaviors related to that experience, behaviors that seem or are believed to somehow moderate or protect from the pain experience.
We have no more reason to doubt the reliable, consistent reports of problem substance users about the drivers and underlying sources of their compulsive behaviors than we do individuals experiencing chronic pain. We have no need or evidence to concoct unsupported theories about diseased brains, or learning, or genetic causes, to explain the symptomatic pain behaviors – we have no reason to doubt the reliable reports of patients experiencing pain and can relate to their reports through personal experience. The same is true for patients describing compulsive substance use.
That’s how we know, from what he hear when we listen well to those in pain, and their reliable reports of how they feel compelled to engage in problem substance use are enough to dismantle essentially everything we have been messaged, hijacked, to believe, falsely, about “addiction”, “hijacked brains”, “addiction medicine”, “addiction treatment” and related lethal fabrications.
Multiple upcoming posts will focus on important treatment implications for the picture we have, established by longstanding evidence, of the nature of problem substance use.